Recent research has revealed a close connection between oral health and overall health.
For example, the epithelial cleft caused by periodontal disease becomes an entry point for toxins released by bacteria within the periodontal pocket, as well as for the bacteria themselves, into the bloodstream. When periodontal disease progresses to moderate or severe stages, the area of this cleft is said to increase from the size of a business card to that of a postcard.
Periodontal disease can exacerbate a wide range of systemic diseases, including diabetes, infective endocarditis, angina, myocardial infarction, chronic obstructive pulmonary disease (COPD), aspiration pneumonia, dementia, rheumatoid arthritis, and preterm birth.
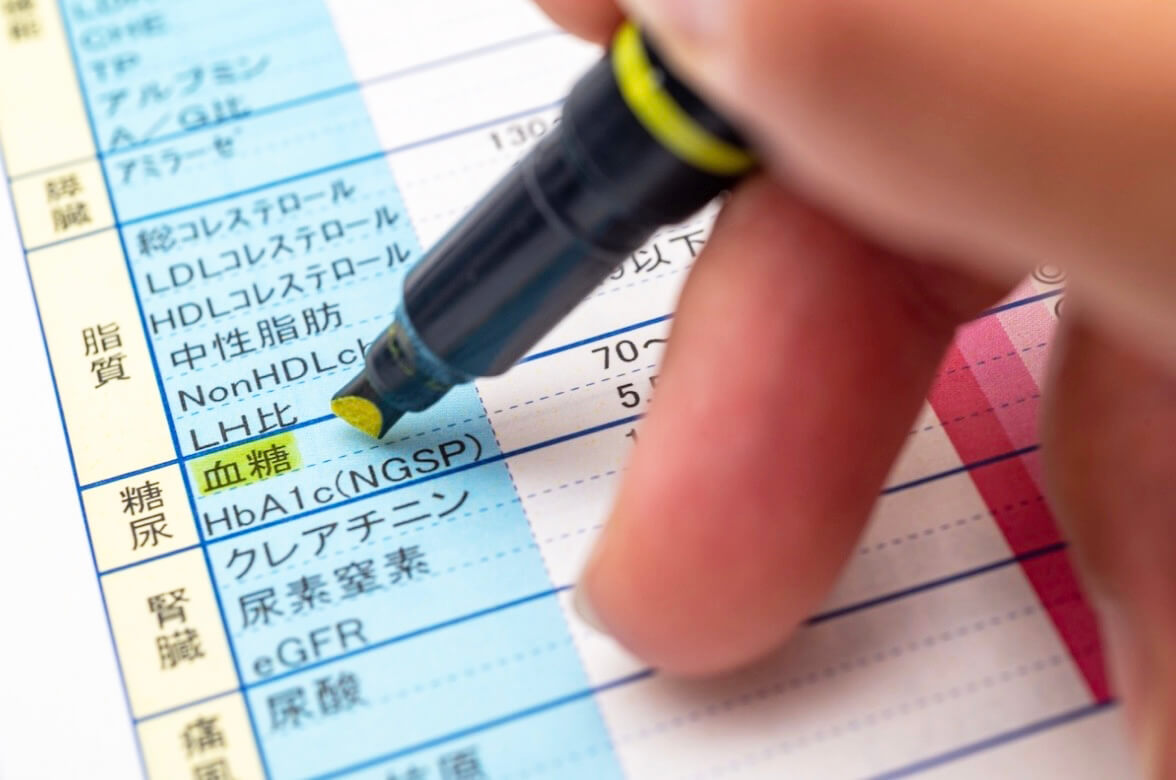
For example, diabetes impairs blood sugar control and facilitates bacterial infection, thereby worsening periodontal disease. Conversely, improving blood sugar levels through periodontal treatment prevents the release of cytokines (IL-6, TNF-α) secreted by immune cells into the bloodstream, leading to improved diabetes management.
Periodontal Disease and Diabetes
Diabetes exacerbates periodontal disease by impairing blood sugar control and facilitating bacterial infection. Conversely, periodontal treatment improves blood sugar levels, thereby preventing the release of cytokines (IL-6, TNF-α) secreted by immune cells into the bloodstream, which in turn improves diabetes.
Periodontal disease worsens type 2 diabetes
Demmer et al., 2008
A positive correlation was observed between the severity of periodontal disease and the onset of type 2 diabetes, indicating that periodontal disease is a predictor for type 2 diabetes onset. Individuals with moderate to severe periodontal disease have a significantly higher risk of developing diabetes compared to healthy individuals.
View academic papers (external site)Periodontal Disease and Coronary Heart Disease
Danesh et al., 2004
C-reactive protein (CRP) levels, an indicator reflecting the degree of inflammation within the body that rises due to inflammation caused by periodontal disease, are used as a predictor for coronary artery disease.
Periodontal Disease and Endothelial Dysfunction
Tonetti et al., 2007
Intensive periodontal treatment induced acute, short-term systemic inflammation and endothelial dysfunction (impaired physiological functions such as immune responses, hemostasis, and vascular tone regulation performed by endothelial cells lining the inner surface of blood vessels). However, six months after treatment, improvement in the oral environment was associated with improved endothelial function.
Periodontal Disease and Coronary Artery Disease
Nakajima et al., 2010
Elevated systemic C-reactive protein levels associated with periodontitis may increase the risk of coronary artery disease.
